Preventable, yet has the highest mortality
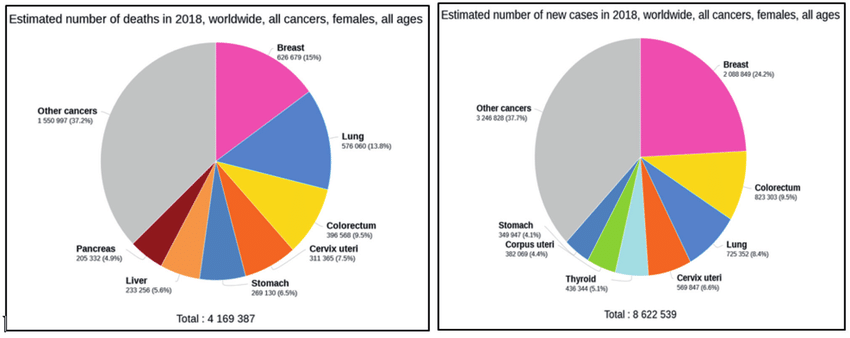
Cervical cancer is one of the leading causes of cancer deaths among women worldwide. Globally, it ranks 4th most common cause of cancer deaths in the female population. In Namibia, it is the 2nd cause of cancer-related death in women, just shy behind breast cancer.
It is caused by persistent infections with the sexually transmitted Human Papilloma Virus (HPV), common in teenagers and women in their early 20s. The risk of developing cervical cancer after HPV infection is higher with cigarette smoking, HIV infections, long term combined oral contraceptives use and immune-compromised states (taken after organ transplants).
Even though cervical cancer is preventable, statistical figures reflect high mortality, mainly due to late diagnosis at advanced cancer stages.
Consistent routine screening, modification of risk factors and treatment for and vaccination against HPV infections are important measures in the prevention of cervical cancer.

– Screening
Pap Smear and testing for HPV are the two screening tests recommended. Pap Smear involves the collection of cells around the cervical opening, which are then examined in the laboratory to check for cells suggestive of cervical cancer or those leading up to its development.
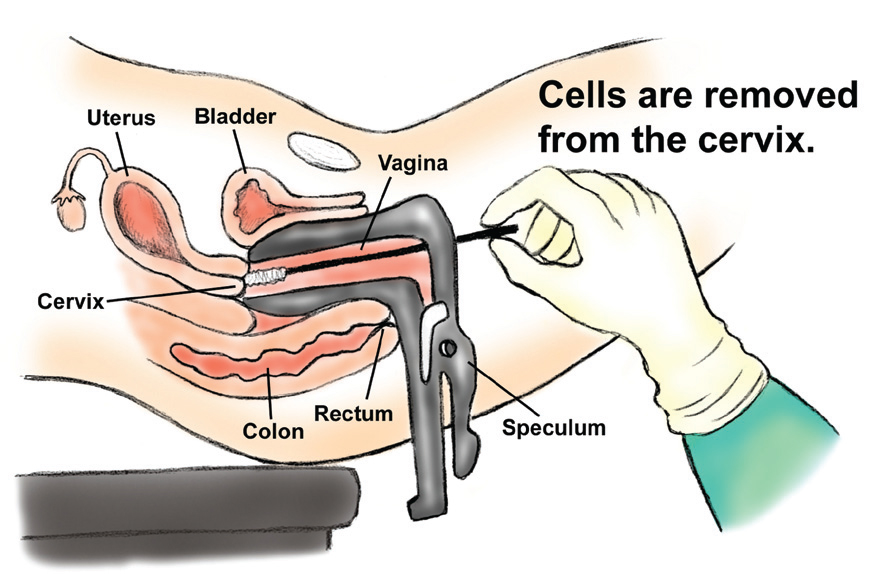
The same method is used to collect the sample to test for HPV. The two tests are either done individually or together i.e. co-testing.
For women younger than 21, preventive strategies like HPV vaccinations and sexual health education are adequate to lower the chances of STI exposure. Only after one turns 21 are they eligible for a screening.
Women aged 21-29 should have a Pap smear done every 3 years. Those aged 30-65 should have both Pap smear and HPV testing (co-testing) done every 5 years or just a Pap smear (every 3 years).
Women vaccinated against HPV should follow the recommendations given above.
– Specific screening guidelines
For women infected with HIV, screening starts as early as the onset of sexual activity, regardless of mode of HIV transmission. A Pap smear is initiated at HIV diagnosis for women below 30 years and it’s repeated annually, and then every 3 years after three consecutive negative annual results. The screening in this population continues throughout their lifetime.
– HPV Vaccination
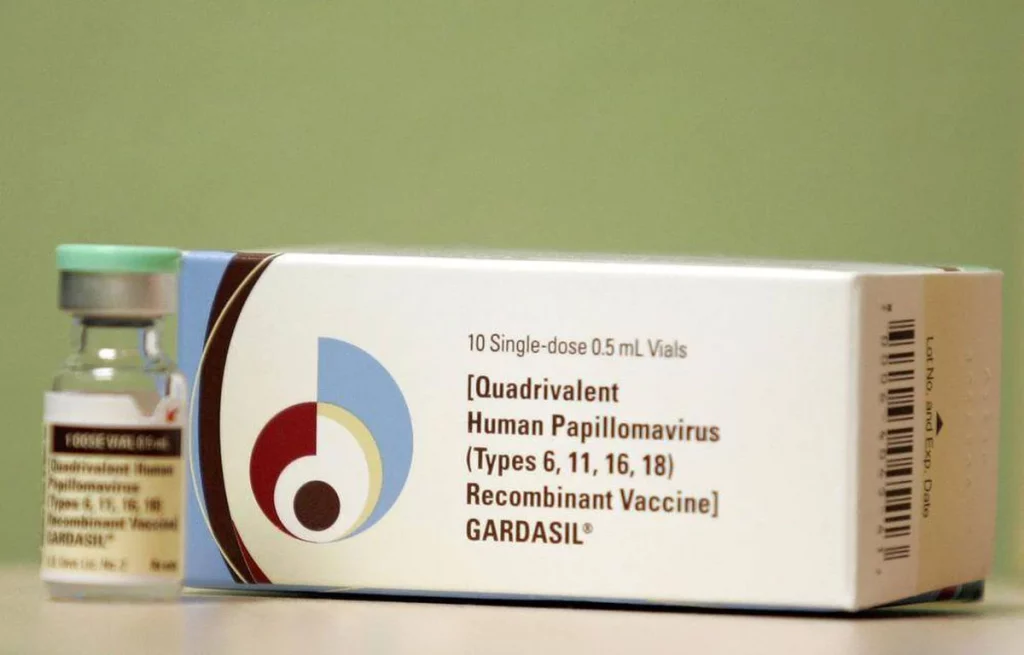
There are three vaccines have been approved for women aged 9-26 years, namely:
- Bivalent vaccine (Cervarix) – covers for HPV types 16 and 18
- Quadrivalent vaccine (Gardasil) – covers HPV types 6, 11, 16 and 18
- HPV 9-valent vaccine (Gardasil 9) – covers HPV types 6, 11, 16, 18, 31, 33, 45, 52 and 58
– Risk Factor Modification
You’re at risk of Cervical Cancer if any of these apply to you:
- Have a family history of cervical cancer
- Have a weakened immune system
- Smoke
- Chlamydia infection
- Long-term use of oral contraceptives (birth control pills)
- Multiple full-term pregnancies
- Young age (<25) when you had your first full-term pregnancy
- Sexual history – became sexually active at a young age (<18 years old) and had/have a lot of sexual partners
Please don’t wait until it’s too late to get screened, ladies! You want to make sure that this cancer is detected early enough and doesn’t stand a chance to fester in your body.